
Abdominoplasty is more than a mere aesthetic problem
Not everyone has drawn the lucky ticket in the gene lottery, where you can wear your Grade 12 jeans a week after giving birth. The bodies of the vast majority of women who have given birth are changing, and sport and a healthy lifestyle cannot always control some of the transformations. We can employ willpower to lose undesired weight, but no amount of self-care can repair bulging abdominal muscles or remove extra skin or stretch marks. That is where plastic surgery may help, and it has lately progressing at enormous pace. New surgical procedures and alternatives are doing wonders.
We talk to a plastic, reconstructive and abdominal surgeon Karolis Černauskis at Gijos Klinikos, about abdominoplasty. He commented on the questions most often asked by women.
It is believed that abdominoplasty is only performed on women who have given birth, after their abdominal muscles have separated (due to diastasis). Is it true? What other patients are candidates for this surgery?
I cannot unequivocally agree with this statement. In reality, abdominoplasty is most commonly done on postpartum women with divided rectus abdominis muscles and sagging, generally stretch mark-damaged, skin on the lower abdomen. But this is not a rule – the applicability of this operation is wider.
An increasing number of patients are coming in for this surgery after losing a lot of weight. These patients develop a lot of loose skin in various parts of the body, including the abdomen. Excess skin folds form, they become dishevelled and injured, and little wounds are formed particularly during the warmer season. Abdominoplasty dramatically improves both physical and psychological quality of life for these patients, and the improvement is absolutely astounding.
Another group of patients has hernias in various locations of the abdomen (navel, white line, post-operative). If an abdominal wall hernia is diagnosed along with excess abdominal skin in the lower abdomen and unsightly scars from previous surgeries, combining hernia repair with abdominoplasty can not only provide a great cosmetic result, but also cure abdominal wall hernias, which can sometimes cause serious complications.
What are the symptoms of abdominal muscle separation?
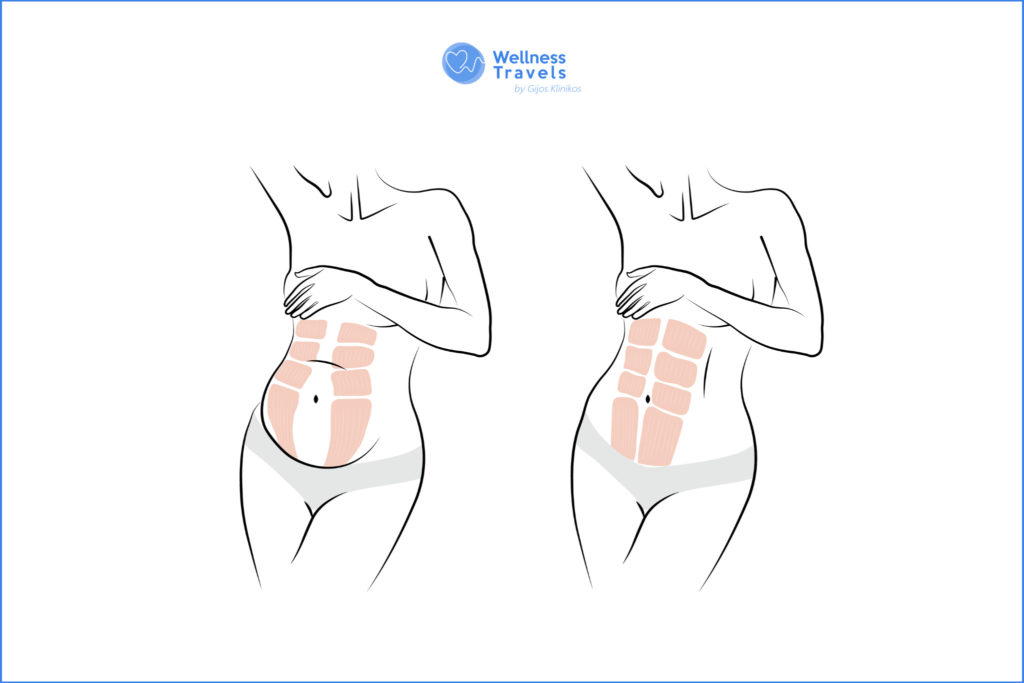
Patients perceive a change in the appearance of their abdomen after having birth. First and foremost, it becomes an aesthetic issue. The abdomen protrudes, is malformed, swells up when you eat, and slimmer women may be able to feel or see the gap between the rectus abdominis muscles. Sagging abdominal muscles are not just a cosmetic issue, but also a significant medical issue. Lower back discomfort and poor posture may be quite uncomfortable. Pelvic muscles weaken, resulting in episodes of incontinence. Sex life is hampered by frequent digestive issues. Hernias are also more prone to develop between separated abdominal muscles.
What causes abdominal muscles to separate? What prevention is there to avoid this?
The most frequent complication of pregnancy is abdominal muscle separation caused by increased pressure inside the abdomen. The muscles separate as the embryo grows and attempts to find room in the abdomen. As a result, the following factors are frequently associated with pregnancy: large foetus, multiple pregnancy, excessive exercise during pregnancy, caesarean section, slim patient. High amounts of intra-abdominal fat, heavy weight lifting, certain connective tissue conditions, and ageing above 35 years are all possible causes. As a result, abdominal muscle separation is not limited to women.
The best prevention is strengthening of abdominal wall and pelvic muscles before pregnancy. Prenatal and postnatal physiotherapy sessions are recommended. It is essential to promote a healthy, balanced diet and to abandon harmful habits.
How is the number of cm of abdominal muscle separation determined? Can a woman “determine” it herself?
Diastasis is determined via a medical check; if two or three fingers “fit” between the muscles, the patient’s abdominal muscles are most likely separated. An abdominal ultrasound can assist to accurately determine the diastasis, its width, and any potential hernias. However, in most situations, the patient is aware that her abdominal muscles are separated prior to seeing the doctor because she feels or observes the above-mentioned symptoms and may feel the gap between the abdominal muscles.
In my clinic, I had to correct 12-14 cm abdominal muscle separations, however, this diastasis was compounded by a complication of massive abdominal wall hernia that included a big portion of the patient’s intestine. This condition necessitates the use of specialised abdominal wall repair procedures as well as synthetic meshes.
What is the connection between hernias and abdominal muscle separations?
The connective tissue membrane, the white line, connects the rectus abdominis muscles. It’s a very strong tissue that keeps our muscles next to each otherr. The pressure within the abdomen rises as the foetus grows, and the white line thins, forcing the rectus abdominis muscles to the sides and creating a gap between them. The thinned white line (diastasis) is no longer as robust as it once was, and abdominal organs might break through it, resulting in hernias. As a result, diastasis and hernias are inextricably related.
What are the problems created by hernias?
Hernias manifest as a bulging mass, a lump in a specific area of the abdomen that we may easily press back into the abdominal cavity with our fingers. The contents of the lump are often abdominal fat, however, in the event of big hernias, abdominal organs such as the intestines may be present. The umbilical hernia is the most prevalent form of hernia in diastasis. Symptoms may not appear right away. Later, especially during exertion, a small lump can gradually grow into a larger lump, causing pain and discomfort. The most hazardous hernia complication is stricture, which occurs when the bulge becomes exceedingly painful and cannot be returned to the abdominal cavity. In this case, urgent surgery is needed, as severe health problems can occur.
What should I be aware of as I prepare for abdominoplasty surgery?
The preparation is fairly simple, but there are a few key points to remember. It is critical to quit smoking and give up other harmful habits. Smoking has a negative impact on post-operative wound healing. Body mass index should not exceed 28. A woman should not consider abdominoplasty until 6-8 months after breastfeeding. It’s also important to attempt physiotherapy and sports first, and only if those don’t work should you consider surgery.
To obtain the greatest cosmetic effect, abdominoplasty can be coupled with other plastic surgery treatments such as liposuction, breast surgery, arm surgery, etc. Preparation for difficult surgery may differ in this scenario. Combinations, on the other hand, are determined on a case-by-case basis, taking into account the patient’s blood parameters, comorbidities, and overall medical condition.
What are the post-surgery recommendations?
When diastasis is corrected after abdominoplasty, it is necessary to wear a specific compression corset or belt for 6-8 weeks. It is vital to avoid exercise activity for several months and to begin training your abdominal muscles only three months following surgery. Massages with lymphatic drainage are advised to minimise post-operative edoema.
 ABDOMINAL SURGERY
ABDOMINAL SURGERY